Endoscopic Retrograde Cholangiopancreatography (ERCP) in Connecticut
What is an ERCP?
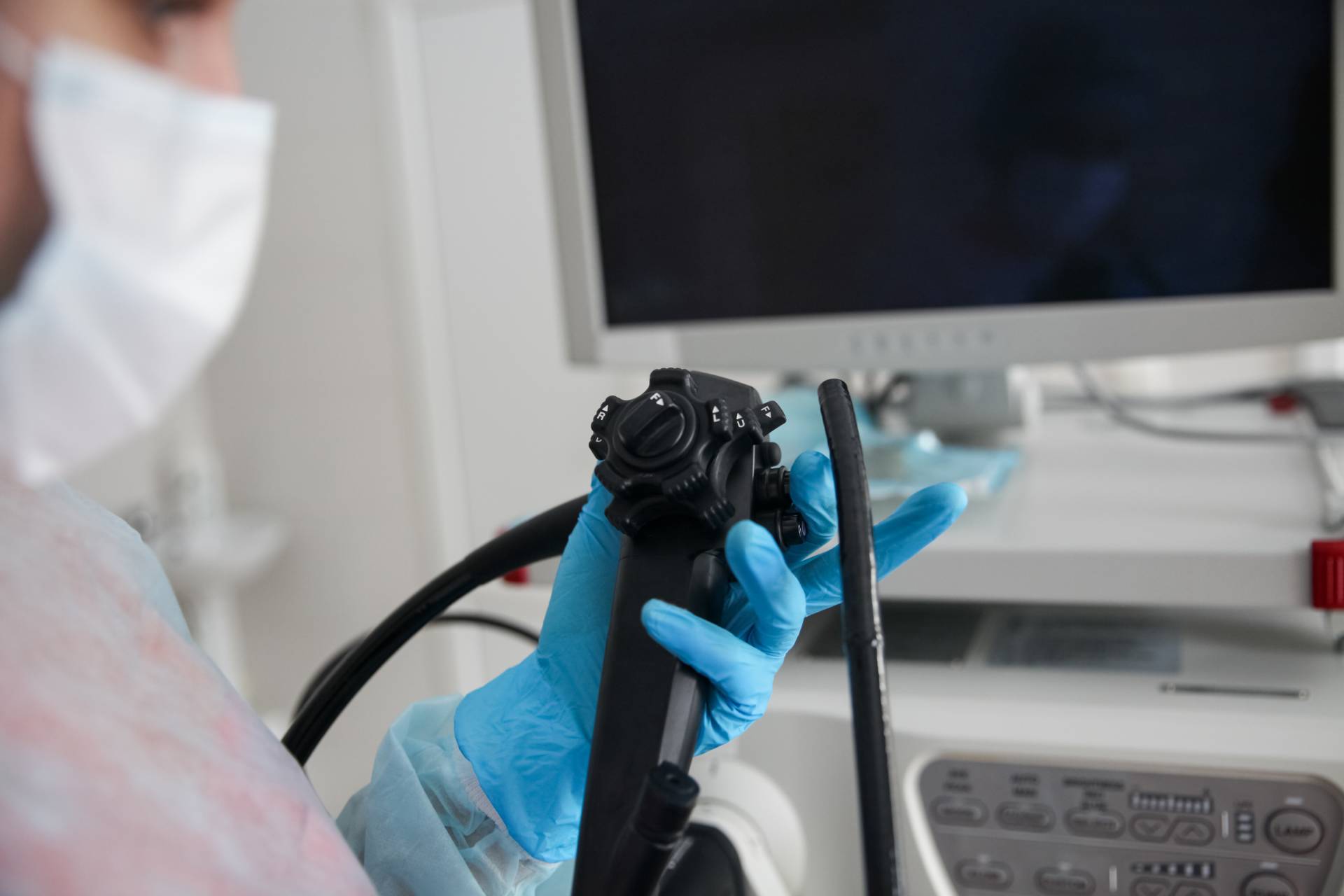
Connecticut GI performs endoscopic tests to evaluate several gastrointestinal conditions in patients. An endoscopic retrograde cholangiopancreatography (ERCP) is an endoscopic process where a slender, elongated tube or “scope” is placed into the oral cavity and gently moved to the duodenum or first portion of the small intestine. The device contains a light and a camera that allows the physician to examine the lining of the esophagus, stomach, small intestine, the entrance to the bile duct, and the pancreatic duct. An endoscopic retrograde cholangiopancreatography test may be recommended to identify the cause of gastrointestinal concerns, including:
- Pancreatitis
- Abnormal x-ray results
- Abdominal pain
- Abnormal liver test
Please call one of our Connecticut practice locations today to request a consultation with a GI specialist to find out more about an ERCP procedure.
What are the benefits of an ERCP?
An ERCP procedure may be recommended if you have abnormal liver results after a blood test, if you have inflammation of the pancreas, or if you notice symptoms such as abdominal pain or discomfort or yellowing of the skin and eyes. Some benefits of an ERCP procedure include:
- Diagnostic and therapeutic: This approach can serve dual purposes, helping gastroenterologists identify diseases or conditions and provide treatment during the same process. As such, this can diminish the need for multiple treatments.
- Reduced recovery times: Patients often have faster recovery times with an ERCP compared to traditional surgical approaches, facilitating a faster return to normal daily activities.
- Enhanced precision: An ERCP helps facilitate the precise visualization of and treatment within the biliary and pancreatic ducts, which is crucial for precision diagnosis and treatment of a condition.
- Efficiency: The ability to detect and treat a health concern during a single procedure commonly minimizes the overall treatment process.
How can I prepare for my ERCP procedure?
Prior to your ERCP, you will be provided with specific instructions from your gastroenterologist at Connecticut GI regarding what to expect and how to prepare. In most cases, you will be able to eat your regular diet the day prior to the test. Patients will be instructed not to drink or eat after midnight except for medications. It is imperative to follow the directions given to you by your provider. Additional information surrounding your medications may be given. In most circumstances, your medication schedule will be followed as normal. However, in certain circumstances, especially in patients on blood thinners (i.e., warfarin, Plavix®, Coumadin®, aspirin, and anti-inflammatories) and in diabetic patients, specific instructions will be provided.
What happens the day of the ERCP procedure?
Our staff will ask you to arrive at the endoscopy center in Connecticut 1 – 1.5 hours prior to your ERCP evaluation. This is to allow time to fill out paperwork and prepare for the exam. You will then need to put on a medical gown. Our clinical team will place an intravenous (IV) line in your arm in order for sedation to be provided. Special equipment will also be used to allow the specialist and staff to monitor your pulse, heart rate, blood pressure, breathing oxygen, and electrocardiogram levels during and after the procedure.
After you enter the treatment room, you will be asked to position yourself on your stomach on the stretcher. The sedation solution will then be administered. Small amounts are given at a time to help ensure that you do not have any reaction to the medication and to provide only the dosage you need individually. Compared to other variations of endoscopic procedures, it is not unusual for general anesthesia to be given for an ERCP procedure. When the necessary level of sedation is reached, the endoscope device will be gently placed into the mouth. The flexible device will be gently moved through the esophagus and down into the stomach and small intestine to the area where the bile duct and pancreatic duct open into the small bowel. A small amount of air is administered via the endoscope into the GI tract to aid in visibility. During an ERCP, radiographic contrast dye is introduced into the bile and pancreatic ducts. An x-ray imaging machine is utilized to take pictures of these structures to determine if there are any abnormalities or concerns. The remaining liquid in the upper digestive tract can be removed by way of the endoscope. Depending on the findings of the exam, several processes may be carried out during the procedure, such as tissue extraction for a biopsy, sphincterotomy (opening the bile duct or pancreatic duct), removal of gallstones from the bile ducts or stones from the pancreatic ducts, or placement of stents (plastic/metal tubes) into the bile duct or pancreatic duct. When the procedure is complete, as much of the remaining fluid and air as possible will be extracted via the endoscope. The ERCP procedure takes between 30 – 90 minutes based on the results.
When the procedure is concluded, you will be taken to the recovery area to be evaluated while the sedation medication begins to wear off. The extent of sedation administered during the test and your body’s response to the medication will determine how fast you wake up, though most people are alert enough for release within 45 – 60 minutes. You will not be allowed to operate any vehicles for the rest of the day and will, therefore, need to arrange for a ride home in advance. You will also be instructed not to perform strenuous activities, work, or sign important documents for the rest of the day. Most people can drink and eat normally after being dismissed from the endoscopy unit, though detailed instructions regarding eating, activity, and medications will be reviewed before dismissal. Occasionally, patients will be recommended for an overnight hospital stay for evaluation or monitoring.
When will I get my ERCP results?
Following the ERCP procedure, the specialist and/or clinical staff will explain the results of the procedure to you. Generally, patients will not recall what they are told after the ERCP process because of the effects of the sedation. Our Connecticut GI team strongly encourages you to bring someone with whom the findings can also be shared. You will also go home with a typed report and will be informed of any biopsy or other test results, usually within one week.
What are the risks of an ERCP?
ERCP, in general, is regarded as a very safe procedure. Most complications are not life-threatening, but if a complication arises it may lead to hospitalization and surgery. Before the procedure, the nursing team will review a consent form with the patient. The provider will discuss treatment risks before the procedure begins, and any concerns or questions can be addressed.
A health issue known as acute pancreatitis, or inflammation of the pancreas, is the most common complication. The condition may affect 5 – 8% of cases, though, depending on individual factors, the risk can run as high as 20%. Pancreatitis signs and symptoms may include nausea, vomiting, abdominal pain, and sometimes fever. Most cases of pancreatitis are mild and require a hospital stay of four days or less. During the hospitalization, patients often only require pain and nausea medications, along with IV fluids. Rarely, however, pancreatitis can be more severe and may be life-threatening.
Adverse medication reactions related to sedation can occur. These can include but are not limited to difficulty breathing, effects on blood pressure and the heart, irritation of the vessel used to administer the sedative, and allergic reactions. Bleeding can result from a sphincterotomy or biopsies. Significant bleeding, such as that which might indicate a hospital visit or a blood transfusion, is highly unusual.
The piercing or perforation of the small intestine, stomach, or esophagus can occur. This may be detected at some point during the ERCP procedure, or it may not be identified until later in the day. In most situations, a puncture of this type will result in hospitalization and surgery. This is not a common complication, even when biopsies are completed or a sphincterotomy is conducted.
Finally, in 5 – 10% of individuals, the exam may not be able to be completed for several reasons. It is extremely important that the patient call the physician’s office immediately if any symptoms arise after the test, such as bleeding, increasing abdominal pain, or fever.
The same as with any other testing process, ERCP is not flawless. There is a small, acknowledged risk that abnormalities, including malignancies, may not be identified during the exam. It is crucial to continually consult with your providers as recommended and inform them of any persistent or new issues or symptoms.
Should you need an ERCP in Connecticut, our GI specialists can help you find the appropriate solution for your healthcare needs.
What are alternatives to an ERCP?
To some extent, any alternative options to ERCP will depend on the purpose for needing an endoscopic retrograde cholangiopancreatography in the first place. For the majority of individuals, ERCP is an ideal option to identify and treat certain problems in the biliary and pancreatic systems. However, an imaging technique known as a magnetic resonance cholangiopancreatography (MRCP), percutaneous transhepatic cholangiogram (PTC), or echo-endoscopy or endoscopic ultrasound (EUS) can also evaluate the biliary ducts and pancreatic ducts. It is important to note that a magnetic resonance cholangiopancreatography is only a diagnostic tool. Addressing any concerns will require an ERCP or a surgical procedure. In addition, percutaneous transhepatic cholangiogram or endoscopic ultrasound do have treatment options.

Exceptional care for endoscopic procedures
ERCP FAQs
What questions might be helpful to ask my GI provider about ERCP?
Should you find out that you need an ERCP procedure, you’ll probably have questions and may be unsure of where to start. Some common questions to ask your GI provider could include:
- What does your gastroenterologist expect to find during this procedure?
- What is the general success rate of an ERCP?
- In the event a complication occurs, are there any signs or symptoms you might experience?
What should you avoid after having an ERCP?
You should not drive for 24 hours after undergoing your ERCP because the anesthesia may take that long to leave your body fully. As such, it is essential to have a friend or family member take you home. Our team may instruct you to avoid eating for a specific timeframe, depending on what form of treatment was performed during the ERCP. Our team may also recommend taking the remainder of the day and possibly the following day off work to recover. Your Connecticut GI team will help you understand what to anticipate before, during, and after your procedure.
What procedures might be performed during an ERCP?
An ERCP allows your GI provider to perform several procedures during an ERCP. Some of these procedures include:
- Placement of pancreatic and biliary stents
- Biopsies
- Stone removal (gallstones in the bile duct)
- Sphincterotomy of the biliary sphincter
How might you prepare for an ERCP?
Our Connecticut GI team can provide you with information on prepping for an ERCP. However, some of the things you might be advised to follow are:
- Do not drink or eat for eight hours prior to your procedure. (Water may be fine. Ask your doctor for confirmation.)
- Avoid smoking for eight hours prior to your ERCP procedure.
- Be sure to give your doctor a list of all medications you are currently taking as well as any allergies you may have.
